Blog
Multidisciplinary Rounds – Not the Only Tool in the Toolbox
Authored by: Bonnie Geld, Shawna Kates, Melissa Ward, Kiandra Florence
The Center for Case Management, Spring 2024

Multidisciplinary rounds (MDRs) are beneficial in keeping patient care at the center while incorporating multiple care team members. MDRs are proven to develop a collaborative approach to care and comprehensive understanding amongst team members, making it an excellent strategy to manage patient length of stay. However, many overlooked strategies can highly impact length of stay management.
MDRs are a highly effective strategy in patient care when there is alignment between team members regarding the care plan and estimated date of discharge. Where LOS efforts often struggle is the employment of a singular tool such as daily MDR, expecting it to problem-solve all barriers. In most rounds today, teams are limited to planning for the day as opposed to “plan for the stay.” It is important to recognize that accompanying strategies must be utilized. For example, the use of scripting for multidisciplinary rounds expands the impact of MDR. Consistent participation and input by essential team members, plus Whiteboard communication at a unit and patient level, are important in translating the plans to the team/patient. A valuable LOS tool is Afternoon Throughput Rounds or “Touchdown Rounds” which are needed to build on the early MDR conversation, hold everyone accountable to their individual action plan, and are the forum with which to escalate and steward any barrier resolution and prevent delays in discharge.
Collaborating with a Physician Advisor to mobilize delays in clinical progression of care, and lead standing collective meetings, such as Complex Care Rounds, (that include CFO, Nursing, CMO, Legal) also influence length of stay planning. Defining, monitoring and sharing KPIs and use of avoidable days data to identify areas of improvement are highly beneficial. Other impactful actions to streamline patient flow include staff training, EMR documentation, communicating medical milestones and estimated date of discharge to patients and families, complex case meetings/huddles, holding higher-level meetings with stakeholders that can “open doors” for solutions to decrease long LOS or patients with complex discharges. Case managers are essential in connecting preferred provider communities and organizations to manage expectations around a timely transition.
The list of LOS reduction efforts is expansive and calls for creative applications – but the important lesson is the need to combine and measure a multidisciplinary and multilayered approach and not rely on only one tool, such as MDR, to create significant success in patient length of stay.
Does your hospital need help with length of stay management? Contact our expert team today.
Addressing Heart Disease Treatment Through SDOH
Authored by: Kiandra Florence
The Center for Case Management, February 2024

Heart disease is the leading cause of death for adults in the United States, according to the American Heart Association. The AHA also reports the risks of developing heart disease are staggeringly higher for Black people, with historical and systemic factors playing a major role. Case management and social work practice focus on providing patient-centered treatment, with a helpful tool utilized being Social Determinants of Health. Here’s how this important screening tool can better address heart disease treatment in the Black community:
- Acknowledging Patient’s Circumstances
SDOH focuses on asking the questions that help providers meet patients where they are. With the ability to identify whether a patient has housing, food, etc., there are better opportunities to ensure patients receive the best care possible for their specific needs. This helps eliminate disparities in treatment.
- Whole Patient Approach
In the Black community specifically, providers must be aware of cultural aspects that may impact the patient’s response or willingness to certain treatments. SDOH helps create a whole patient approach by deciphering between what’s relevant and appropriate for the patient at hand.
- Individualized Care
Heart disease is one of the most taxing diagnoses anyone can have, and the care received during treatment must be not only quality but as individualized as possible. What does it look like? Seeking to understand the patient, with empathy and compassion, as a person outside of being a patient. Helping the patient understand their diagnosis and providing ways they can improve their health in simple steps.
- Resources That Work
Providers should seek to care about the patient’s well-being post-inpatient care. One of the most important ways to do so is by connecting the patient with the right resources. When working with the Black community, the provider must take time to find resources that are welcoming and aware of the population they’re taking care of. Implementing proper SDOH helps make this process seamless by fostering an understanding of the patient and their specific needs (financially, socially, and mentally), and ensuring they’ll be able to receive the care they need.
Are you looking for interim leadership in your hospital system? We can help! Contact our team today.
CFCM Leadership Spotlight: Mary Daymont
The Center for Case Management, Winter 2024

Mary Daymont, MSN, RN, CCM, FAAN is a strong case management leader with exceptional expertise and experience linking case management outcomes to revenue outcomes. Her keen focus on mission and margins (ensuring high outcomes are achieved) makes her a coveted leader in hospital systems. Her previous work includes reducing DRG excess days leveraging embedded care pathways, with treatment plans and exit strategies developed as soon as patients are admitted. She was instrumental in transforming the end-to-end Revenue Cycle at her previous employer, Children’s National Medical Center, resulting in a 66% net patient revenue improvement!
With a background in Public Health, Mary has implemented universal Social Determinants of Health across enterprises at all points of entry that immediately linked patients to resources. She continues this work with passion and vigor in working towards achieving health equity. Mary places high importance on transformative leadership, building diverse teams that are engaged, resilient and agile. This has led her to have high retention rates and a team that truly values their work. She translates her incredible leadership skills as an educator for groups and leaders, making her an often sought-after national speaker.
Are you looking for interim leadership in your hospital system? We can help! Contact our team today.
Improving Quality of Life Through Population Health
Authored by: Kiandra Florence, Patty Northern, RN, MBA CCA
The Center for Case Management, November 2023

Population Health is a key ingredient in the care continuum, ensuring wholesome care is given. At The Center for Case Management, we believe Population Health is no longer an option—especially with decreasing reimbursement from payers.
One of our Population Health expert consultants, Patty Northern, RN, MBA CCA, has a heart and passion for increasing patients’ quality of life through collaborative efforts. Patty started in case management as Director of Population Health, comprised of Care Coordination, Quality and Population Health initiatives.
During Native American Heritage Month, with her current work in the Native American population, we discussed Patty’s first-hand knowledge of the benefits of integrating population health into case management.
How does Pop Health tie into case management/care continuum/care transitions/complex care…
Patty: Population Health is required as part of contract negotiations with private payers along with APM payments and ACO/Medicare Shared Savings Program. This entails that Transitions of Care are identified early (time of admission) as well as Chronic Care Management to avoid repeat hospitalizations. If transitions aren’t identified early, then the risk of readmission increases, thus exposing hospitals to readmission penalties that erode their fiscal health and, in turn, decrease resources, staff, and technology to best care for mutual patients.
On the need for warm hand-offs/community relationships/collaborations…
Patty: The core component of Case Management/Care Coordination is having collaborations with internal and external agencies so that resources and knowledge can be shared. I recently had an elderly patient who was going to be homeless and had nowhere to go. Case Management worked with a Senior Services Social Worker to find a group home but wouldn’t take the patient with diabetes insulin SQ. Case Management worked with the provider indicating the A1c’s have been stable, and the patient could go to Group Home if diabetes medicine changed to oral. The provider changed the meds, and the patient is now living safely in the group home. A happy ending for sure!
November is Native American Heritage Month, and you’re currently working with the Native American Population. Why is care coordination, as it pertains to Pop Health, important for the Native American/Indigenous population?
Patty: Care Coordination is becoming a key player in the Value-Based Care (VBC) Model in which CMS is moving from Fee for Service (FFS) to VBC reimbursement. That entails that providers, facilities, etc. are responsible for ensuring quality of care is given and not just a service. Providers/facilities are evaluated on health care outcomes and reducing health care fragmentation. The Native American population has a higher incidence of Diabetes, Congestive Heart Failure and Liver Disease than other races, making Care Coordination instrumental in reducing hospitalizations while increasing quality of life.
On SDOH and CMS 2024 New Requirements…
Patty: In the past few years, CMS has recognized that SDOH has a direct impact on physical health. If these SDOH gaps can be assessed and addressed, this will help promote quality of life and decrease unnecessary ER and INPT admissions. CMS recognizes the importance of increased reimbursement for providers/facilities that address SDOH because, in the long run, it helps CMS keep patients out of the hospitals and extend healthcare dollars.
What are some specific SDOHs needed to serve the Native American population better?
Patty: The largest SDOH factor for Native Americans seen is literacy. This population averages a 9th-grade education, so understanding their disease processes and treatments can be challenging. Another SDOH factor seen commonly is Housing Instability. Most of this population lives in dwellings that are not inhabitable or stay temporarily with friends and family. Available housing is very limited on the reservation, and if they move off the reservation to obtain housing, they can lose their tribal benefits. Most of the time, they choose homelessness over losing benefits which directly impacts their physical health.
Any wins you’d like to share…
Patty: We have a case manager with a complex dialysis patient who lives in an SNF and has dialysis three times/week, which is all covered by Indian funds. The patient needed wheelchair transportation to get back and forth 3x/week, but the department responsible for approving these funds was hesitant to approve them. It was a battle for a week until I had to speak up and showcase the value of Case Management. I explained that a missed dialysis appointment would send the patient into Fluid Overload and would need to go to the ER for dialysis. Ultimately those very sick people end up getting admitted for Altered Mental Status, electrolytes WAY off, wet lungs, cardiac side effects, etc. The point was made that a $40 trip each way to dialysis will ultimately avoid a $20K hospital admission and provide quality care for the patient. The rides got approved and avoided unnecessary hospitalization.
Does your case management department need support with population health and capacity issues? We can help! Contact our team today.
Breast Cancer Awareness Month
Authored by: Kiandra Florence
The Center for Case Management, October 2023

The American Cancer Society reports breast cancer as the most common cancer diagnosis among women in the U.S., with 1 in 8 women diagnosed in her lifetime. As a health organization, partnering with your case management department is vital in ensuring patients diagnosed with breast cancer receive the best resources and quality of care available to them. Here’s what that could look like for your organization.
Identify Patient Needs
Patients with breast cancer diagnosis experience a myriad of emotions, concerns and life changes that vary depending on factors such as the patient’s ethnicity, age and support system. Your health organization’s case management team is equipped to find out everything your patient needs (from psychosocial to financial support) in their journey.
Advocate for Patient/Family
With a breast cancer diagnosis, patients truly benefit from having a case manager available to advocate for their and their family’s needs. This may look like communicating with members across the care team to ensure proper medication, education and support are made a priority, depending on the exact needs of the patient. Our case management experts go the extra mile to make sure patients are receiving equitable and inclusive care.
Seek Resources That Make the Patient/Family as Comfortable as Possible
Breast cancer impacts patients differently, this is why a case manager is an invaluable resource to have on a patient’s care team. Case managers push for accessibility to hospital and community resources that make the patient’s care as affordable and comfortable as possible.
Ready to upgrade your case management department? Consult our team of experts to learn about our case management assessment options. Contact us today!
Communicating Your Value: The Case Manager’s Guide
By Dr. Colleen Morley, President of CMSA, and Bonnie Geld, MSW, President and CEO of CFCM
For too long the case management profession has been referred to as healthcare’s best kept secret. No more.
The Case Management Society of America (CMSA) and The Center for Case Management (CFCM) have worked together to present their collaborative Position Paper Communicating Your Value: The Case Manager’s Guide. This first-of-its-kind paper highlights invaluable information on wide-ranging case management roles and features insight from some of the best and brightest case managers in the field. CMSA and CFCM look forward to raising awareness about the undeniable impact case managers have on the healthcare continuum.
With yesterday’s official launch, we sat down to discuss this special collaboration.
On how this collaboration came to be…
Colleen: I have long been a fan of CFCM and Karen Zander and had the opportunity to meet Bonnie at a conference. When I was looking for entities to collaborate with, CFCM was top of my list! In my usual overly exuberant way, I am so incredibly excited about this project, from working with CFCM to the subject matter experts who volunteered their time, talents and perspectives in their contributions to the opportunity to publish something that I have been longing to see; why is case management important, in case management’s own words!
Bonnie: Other than a mutual admiration for CMSA/CFCM, Colleen and I had the opportunity to connect and discuss our common goals for Case Management and Social Work Practice. We found that our organizations align towards improving the visibility of the value of this discipline. Writing this paper was a wonderful experience and an honor. We had the opportunity to learn from so many professionals in the field. The value is clear!
On why it is important to discuss case management’s value and why it was important that the Communicating Your Value: The Case Manager’s Guide Position Paper be shared now…
Colleen: Because we are the best kept secret in all of healthcare and we are on a mission to break that perception. It’s time case management took its place in the light and that the entire healthcare community, including the patient/caregiver, understood the value a professional case manager brings to their journey.
Bonnie: October is Case Management month. This paper offers another opportunity to highlight the importance and value of these professions. Hospitals and Health Systems don’t always have a clear understanding of the case management practice; nor do they leverage the skill sets of these clinicians so that true care coordination and patient progress can be achieved. We believe our paper highlights the value case managers bring to the organization and to the patients and communities they serve.
On what they hope to accomplish…
Colleen: We hope to start conversations about where case managers “should be” in the healthcare continuum (answer: everywhere) and how they are, not just integral but invaluable members of the healthcare team, regardless of practice setting. We also want to inform patient/caregivers about who we are, what we do and how they benefit from us (and the services we provide).
Bonnie: Value begins with visibility. We believe that this position paper offers more visibility to demonstrate our worth and reminds the health care ecosystem that we are an essential piece of the care continuum.
Download your FREE copy of Communicating Your Value: The Case Manager’s Guide here: https://tinyurl.com/4sdk25w6
Having Confidence in End-of-Life Conversations, Hospice and Capacity Management
Authored by: Melissa Ward, RN, BSN, MSN, Kiandra Florence
The Center for Case Management, July 2023

Holding Hands with Elderly Patient — Image by © Wernher Krutein/Corbis
End-of-life conversations are significant but difficult to have, especially in hospital settings. Our experts find that hospital clinic teams often struggle to discuss end-of-life care with patients (primarily due to limited knowledge). As end-of-life care is vital for case management departments in managing hospice and capacity management, we sorted through best practices for bringing end-of-life care options to the forefront.
Educating your clinical staff on the benefits and options available to the patient and family is one of the best ways to approach end-of-life care. When your hospital team feels equipped and knowledgeable, they’re more apt to approach end-of-life conversations head-on. By keeping your team up to date with resources and information, there’s confidence in their discussions with patients.
Having end-of-life care conversations as early as possible can improve your hospital capacity management issues. Many hospital teams mistakenly address end-of-life care options too late, making it unfeasible to move the patient. The sooner you can address care opportunities, the quicker the patient and family can decide and potentially open the hospital bed.
The impact of not discussing end-of-life care extends beyond the patient. In hospital settings, if patients are admitted and expected to pass away, they require an intensive level of care, medication and support. When billed, these costs can be astronomical for families and organizations if there are no monies available post-death. Hospice costs are typically covered by most private insurance and are covered by Medicare/Medicaid. Death and dying are emotionally difficult for families as well; with hospice—support extends beyond the hospital.
Here are strategies to improve your hospital’s clinical team’s end-of-life care approach:
- Implement end-of-life education for staff in the onboarding process.
- Create a structure for how to introduce end-of-life care discussions.
- Know who to contact.
- Learn about the benefits (i.e. Hospice, types of resources available, options across different cities).
- Seek community partnerships with hospice agencies.
- Partner with Physician Advisor for support with providers.
Does your case management department need support with end-of-life care and capacity issues? We can help! Contact our team today.
Women Who Shaped Social Work
Authored by: Kiandra Florence
The Center for Case Management, March 2023
This Women’s History and Social Work Month we celebrate brilliant social work leaders who changed the pioneered social work the way we know it.
-
Frances Perkins – Her social work career led her to become the first woman to serve on the New York State Industrial Commission and make a name for herself in politics. By the time she was appointed Secretary of Labor by Franklin D. Roosevelt, she brought three decades of commitment and experience to social reform. She was the first female Cabinet member; the first woman to enter the presidential line of succession. Her work and dedication helped change the 58-hour work week for women to 48 hours! She fought for a minimum wage law and helped draft the National Labor Relations Act, the Fair Labor Standards Act, and the Social Security Act.
-
Grace Abbott – Grace had a passion for bettering immigration laws. Her work with the Immigrants’ Protective League led to her involvement in securing protective legislation, her studies of conditions at Ellis Island, and her testimony before Congress against immigration restrictions. During her social work career, she was appointed a professor of public welfare at the University of Chicago’s School of Social Service Administration. In 1934–35 she helped plan the social security system as a member of President Franklin D. Roosevelt’s Council on Economic Security, and she was a U.S. delegate to the International Labor Organization in 1935 and 1937.
-
Julia C. Lathrop – Julia utilized her advocacy for the mentally ill, immigrants, equal rights for women, social reform, and child welfare to enforce change. She worked with the Illinois Board of Charities, where she visited facilities for the mentally ill, sick, and disabled in the Chicago area. She advocated that separate facilities should be established that would attend to these specific groups. In 1912, she became the first appointed woman bureau chief in the federal government when President William Taft asked her to join the Children’s Bureau. Her work as chief emphasized the importance of issues like child labor laws and juvenile delinquency. In addition, during her tenure as chief, the Children’s Bureau’s budget increased tenfold and the effort to reduce the nation’s high infant mortality rate resulted in the 1921 Sheppard-Towner Maternity and Infancy Act. By 1921, becoming the first federally funded social welfare measure in the United States.
-
Alice Salomon – In Germany, she is acknowledged as one of the founding mothers of social work, particularly social work education. She directed the first full-time course of social work in her native city, Berlin, initiated and chaired the national conference of schools of social work in Germany, and altogether was among those who developed one of the earliest continuing education programs. She was among the initiators and first president of the International Committee of Schools of Social Work. During her teaching career, she wrote twenty-eight books and more than four hundred articles, many on international and intercultural issues.
-
Jane Addams – In 1889, Addams helped found Hull House in Chicago, the first settlement house in the United States. The goal was for educated women to share all kinds of knowledge, from basic skills to arts and literature with poorer people in the neighborhood. Jane leveraged her social skills to expand her efforts to improve society. Along with other progressive women reformers, she was instrumental in successfully lobbying for the establishment of a juvenile court system, better urban sanitation and factory laws, protective labor legislation for women, and more playgrounds and kindergartens throughout Chicago. Jane led an initiative to establish a School of Social Work at the University of Chicago, creating institutional support for a new profession for women. She was active in the women’s suffrage movement as an officer in the National American Women’s Suffrage Association and pro-suffrage columnist. She was also among the founders of the National Association for the Advancement of Colored People (NAACP). In 1931, she became the first American woman to receive the Nobel Peace Prize.
-
Mary E. Richmond – Mary Richmond was known for her ability to organize communities, her development of casework practice, as well as her ability to teach and speak intelligently on a variety of subjects. Mary frequented research, developing what she labeled ‘social diagnosis’. Her famous circle diagram visualized the correspondence between the client and the environment. Her research helped identify six sources of power that are available to social workers and patients: sources within the household, in the person of the client, in the neighborhood and wider social network, in civil agencies, and in private and public agencies. According to Social Welfare, Mary’s book Social Diagnosis (1917), constructed the foundations for the scientific methodology development of professional social work. She searched for the causes of poverty and social exclusion in the interaction between an individual and his or her environment. For her contributions, Mary is considered a key founder of the profession of social work and the importance of professional education.
-
Thyra J. Edwards – A woman of color, Thyra pushed passed all social and racial barriers to effect change in America. She had an international approach to social work and viewed her journalistic work, travel seminars, speaking engagements, and union organizing as a part of her role as a professional in the social work arena. By the end of World War II, she was the executive director of the Congress of American Women. Thyra was a major advocate for the plight of women and children. In 1953, she organized the first Jewish childcare program in Rome to assist children who had been victims of the Holocaust. It’s been stated that, from her point of view, social work should: advocate for disadvantaged and at-risk populations; focus on issues and problems specifically affecting the well-being of women; and demonstrate the ability to work with diverse populations.
-
Grace Coyle – Grace worked extensively in settlement houses and the YWCA, but found a true passion in social work research and education. Her writings and speeches at institutes contributed to the acceptance of group work as a social work method. Grace saw commonality in case and group work, seeking to bridge the gap between the two in an effort to provide better quality services to patients. She argued that group workers needed to become more aware of personality issues and family relationships, while at the same time case workers needed to be more knowledgeable of group dynamics and the use of leisure activities. It was also her belief that a better acquaintance with case work by group workers would reveal the therapeutic possibilities of a group experience. She was a professor of social work and social sciences, developing the first group work course taught at Western Reserve University in Cleveland. Grace was the president of the National Conference of Social Work in 1940, the president of the American Association of Social Workers in 1942 and the Council on Social Work Education from 1958 to 1960.
References: NASW Foundation, Jewish Women’s Archive, WomensHistory.Org, Virginia Commonwealth University
CFCM Interim Director Leadership Services
Authored by: Kiandra Florence
The Center for Case Management, Fall 2022

📸Pictured above: Our Director of Clinical Services, Melissa Ward, MSN, BSN, RN (right), with our interim Debbie Zeveney (left) on a client visit.
The Center for Case Management consultants are industry leaders in case management, with a team of consultants representing the best of the best in healthcare. Our interims are subject matter experts in all areas of case management and social work practice. Partnering with your leaders, our team members work with care to effectively meet the needs of your healthcare organization—at the frontline, and in leadership.
Our Interim Director services offer opportunities in the following areas and more:
- Leadership during periods of transition and instability promoting cultures of excellence
- Effectively managing the day-to-day operations of the department
- Leading Process Improvement and Organizational initiatives as relates to Case Management
- Assistance in the recruitment, interview, and onboarding of permanent leadership
- Strategic planning & setting course for long-term stability and groundwork for a permanent director
- Identifying and supporting Educational needs
- Mentorship and leadership/staff development
- Developing and leading the team(s) to promote best practices in evidence-based care models
- Promoting visibility and collaboration with other leaders and interdisciplinary teams
Are you interested in our interim director services? Contact our team today!
5 Things We Learned (and Still Apply) from the 1940s U.S. Cadet Nurses
Authored by: Kiandra Florence
The Center for Case Management, June/July 2022

While the U.S. Bureau of Labor Statistics projects 194,500 average annual openings for registered nurses and employment growth at 9% in the next 10 years, there was a time in America when the call for nurses was greatly desired. In the early 1940s, the U.S. was experiencing a nationwide nursing shortage due to World War II. The United States Cadet Nurse Corps (CNC) were created in 1943 to help, with the program extending its benefits to women of all races between the ages of 17-35. According to the National Women’s History Museum, those accepted into the program received tuition, cadet uniforms, and a monthly stipend. By the end of the CNC program in 1948, over 124,000 women graduated from nursing school and became Cadet Nurses.
In addition to recruiting and training young women, we owe a lot of credit for the transformation of nursing education—including Public Health Nursing—in the U.S. to the Cadet Nurse Corps. The funding that was provided through the Corps allowed nursing schools to build modern facilities, upgrade laboratory equipment and helped to integrate nursing programs that had previously accepted only white students.
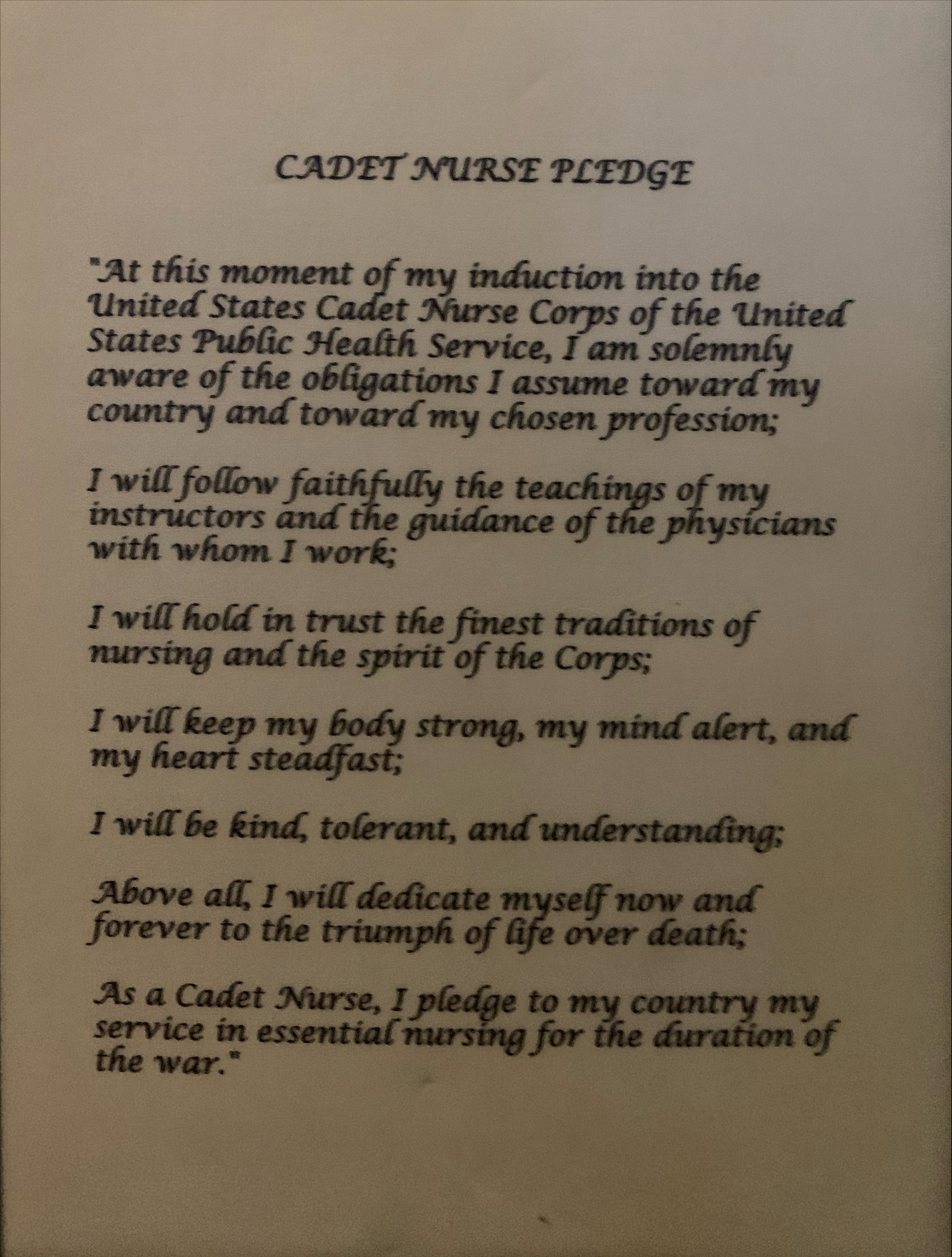
We recently had the privilege of visiting the Public Health Museum in Tewksbury, Massachusetts. During our time at the museum, we reflected on the “Cadet Nurse Pledge” and the work of each nurse in the CNC program. Here’s what we took away:
- Nurses are always at the forefront of the battle against communicable diseases—from the Spanish Flu to COVID-19.
- Nurses remain essential, working to ensure everyone has access to prevention, treatment and rehabilitation.
- Case Managers are today’s contemporary Public Health Nurse.
- Nursing education and inclusion are essential to the growth and development of the profession.
- Nurses work with strength, compassion and integrity.
Are you interested in our nurse case management services? Contact our team today!
Mental Health Awareness Month: Utilizing Case Management in Mental Health Treatment
Authored by: Kiandra Florence
The Center for Case Management, May 2022

The CDC reports that 1 in 5 American adults experience a mental illness in their lifetime. The global pandemic added grief and stress that contributed to the increase in mental health issues such as anxiety and depression. As healthcare professionals see a rise in patients with psychosocial issues—it is important to involve case managers that can help manage these issues.
Assessing Patient Needs
Case managers assess patients to ensure their needs are being met. When mental health concerns are prevalent, patients need specialized care to make sure the issues are being addressed and, most importantly, they are being educated on the best support available to them. With the proper assessment tools, case managers guide the patient to the resources most beneficial to them.
Creating a Treatment Plan
Having the right resources and tools, case managers take a look at areas in the patient’s life that cause stress and offer solutions to help them manage their day-to-day. Developing the best treatment plan is especially important for patients that experience mental health issues. Case managers are equipped to address the areas in a patient’s life that may trigger the mental health concerns–such as work/life balance and financial issues. Working alongside the patient and their families/support systems, case managers discuss options readily available to patients and educate them on how said options meet the patient’s needs.
Putting the Pieces Back Together
Case managers strive to ensure people are making the best use of the mental services available to them. Taking an individualized approach to how the patient is treated, case managers help establish goals and develop strategies that focus on the improvement of the patient’s mental health.
In hospitals and other healthcare settings, case managers are here to help. With continued advocacy for awareness and education, there is hope for improvement in psychosocial patient treatment.
Contact our team to find out more about our case management and psychosocial support services.
Case Management and the Emergency Department
Authored by: Kiandra Florence, Heidi Rohloff, RN, BSN, MSN, ACNP
The Center for Case Management, March/April 2022

Photo Courtesy: iStock
As emergency departments face overcrowding issues, patients are experiencing exaggerated wait times—often overlooked due to capacity limits. Hospital-wide staffing shortages and burnout also contribute to poor quality patient care and hospital flow; leaving many wondering how the system can be improved. At The Center for Case Management, we believe the first step in addressing major ED concerns is implementing best practice case management assessments.
Heidi Rohloff, Nurse Practitioner in Emergency Medicine and CFCM Consultant, has a firsthand look at the poor outcomes currently associated with problems emergency departments are experiencing. ED staff are finding limited beds to be a dominant challenge, especially with the increase of sick patients.
“I had a patient in the ED from October 1st to the second week in December—that’s over 60 days,” Rohloff shared.
According to Rohloff, prolonged periods of hospital stay prevent many patients from receiving beds and adequate care. Patients staying for lengthened amounts of time are often exposed, and made vulnerable, to other illnesses—causing more concerns for ED staff.
“Increased referrals to the ER make it difficult to provide the best patient care,” Rohloff stated. “Case management is key to assessing patients and their care needs.”
Case managers facilitate and assess opportunities for patients by creating sustainable discharge plans. Improved case management practices, such as linking sustainable transitions, provide high-utilizer interventions and help dissipate readmissions alongside the nurse and care coordinator teams. These implementation services ultimately help create effective plans and solutions for patients who are huge utilizers of the ER.
Utilization management is another key component in improving challenges seen in the ER. Utilization nurses take a “big picture” approach to patient care. Together, case managers and utilization nurses pull resources and information needed to determine whether patients should be kept in the ER or provided better alternatives.
“Providers are doing the best they can with the current circumstances, but there are ways in which improvement can be made,” said Rohloff.
As challenges in the ED continue to arise, the need for restructuring and streamlining case management practices to improve patient flow is greater than ever before.
Are you looking to improve your health organization’s outcomes? Contact our team to find out more about our services.
The Benefits of Utilizing Case Management and Social Work: Addressing Heart Disease
Authored by: Kiandra Florence
The Center for Case Management, February 2022

According to the CDC, one person dies from cardiovascular disease every 36 seconds in the United States. During American Heart Month, we work toward increasing awareness about the statistics related to heart disease and ways to prevent it. In hospital systems, case managers and social workers play an important role in helping patients improve their cardiovascular health. Here’s what we know:
Social Workers and Teaching Patient Coping Skills
The role of the social worker is to help people solve and cope with problems in their everyday lives—and that’s no different when it comes to heart health. Managing stress levels is one of the best ways to reduce the risk of heart disease. It is especially important for women to pay attention to their stress as heart disease is a leading cause of death for women in the United States. Social workers aid individuals in identifying the stressors in their lives, providing effective coping skills to prevent heart disease and issues related to those stressors.
Case Managers and Providing Awareness
Case managers seek to organize, facilitate and help others find the best care and solutions for their health. With heart health, case managers can provide patients with tools to recognize symptoms of heart disease before it progresses. Heart disease is easier to treat when patients recognize the signs early. Case managers provide the proper education for detecting heart problems and ways to communicate those issues to others.
This article is dedicated to Beverly Teneholz.
Are you interested in learning more about our case management and social work services? Contact us today.
The Intersectionality Between Healthcare Technology and Patient Care:
Bridging the Health Inequities Gap Through Improved Data Systems
Authored By: Jeffrey Echternach, MBA, AS, NRP, DSC, Kiandra Florence
The Center for Case Management, January 2022
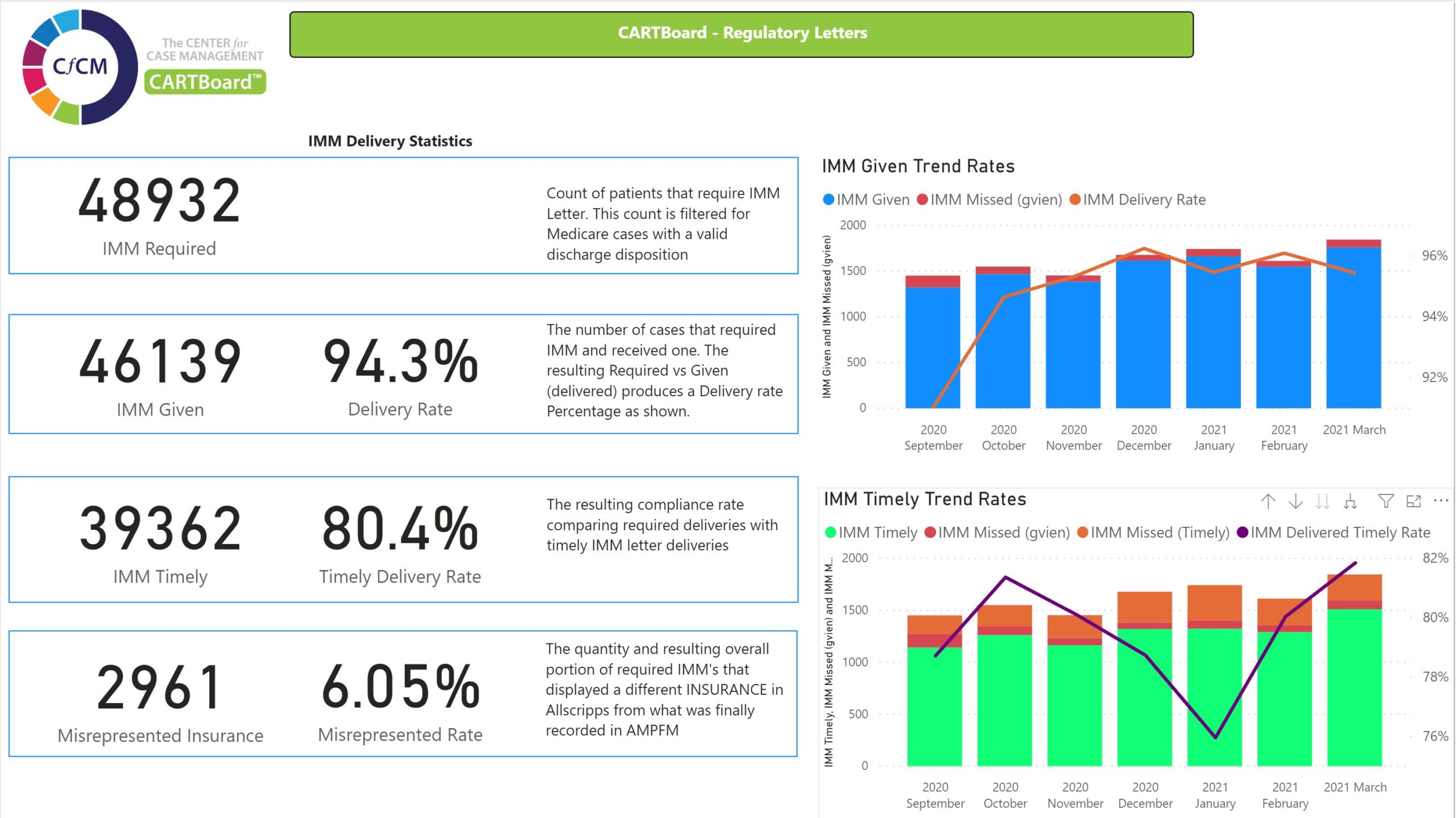
CARTBoard™ is an advanced healthcare data system that provides efficiency scores for hospitals and health systems.
As hospitals look towards solutions for improved patient care, The Center for Case Management is utilizing their data system—CARTBoard™—to develop outcomes and help close the gap on health inequities.
CARTBoard™ is an advanced healthcare data system that provides efficiency scores for hospitals. Jeff Echternach, Technology Officer for The Center for Case Management, said he and the CFCM team developed the system with the priority of improvement of patient outcomes.
Echternach believes that with proper insights and data can, hospitals can identify and bridge the gaps within their health organizations—leading to positive change.
“CARTBoard™ provides health systems with the analytics that point them in the direction they want to go in,” Echternach stated. “The system allows health systems to streamline data and find ways to help their hospitals standardize to the same methodology—resulting in assessing patients properly and providing the best care.”
With the proper process and technology involved, patient identification can be streamlined to ensure potential risk factors are assessed and that patients are receiving resources and information relevant to their case—beginning with screening questions.
Patient responses to screening questions can help identify if a more in-depth questionnaire is needed. After responses are added to medical records, they can then be delivered to the appropriate screening individual (social worker, case manager) for further assessment.
For example, Patient A (facing homelessness) and Patient B (stable home-life) visit the same healthcare provider for flu-like symptoms. If the healthcare provider approaches Patient A and Patient B in the same manner but is unaware of Patient A’s situation, the healthcare provider might miss the opportunity to provide Patient A with adequate care.
Screening tools can start with simple, social determinants of health scale featuring categories that determine whether a patient is safe and stable—leading to counsel and resources that will help them. The more information and details obtained, the better chance of creating a proper discharge plan.
“A hospital discharging a patient that has some limited mobility and a bad heart failure diagnosis, and during screening, says there is a financial concern—the provider should try to address those gaps,” said Jeff Echternach.
After measuring the social determinants scale, results can then be converted into an aggregated score that helps to communicate any risks involved. Echternach said that offering solutions—such as charity medication—could help patients experiencing struggles such as financial issues. However, the best way to know if a patient needs help is by asking the right screening questions. Outside of financial concerns, patients’ needs can range from transportation to housing resources.
According to Echternach, taking the risk scores and stratifying higher scores and lower scores can help determine outcomes for populations. For example, looking at patients that have a very high-risk score in homelessness, a health system might want to know how those patients rank on their acute hospital length of stay. Hospitals could also look at how that score might compare to a population that has a lower score.
Taking it a step further, risk score data enables health systems to see how their various hospital populations compare, discovering what they can do differently to improve outcomes and patient care at other hospitals.
As hospitals face internal challenges, such as staffing shortages, workflow systems can equip case management and social work departments with the best tools for responding and scoring effectively.